Organization
Centre for Disability in Development (CDD)
Location
Seven districts, namely Dhaka, Gazipur, Narayanganj, Patuakhali, Chattogram, Cox’s Bazar and Moulovibazar in Bangladesh
Duration
March 2021 – May 2022
Target group
Persons with disabilities; organizations of persons with disabilities (OPDs) and disability-specific organizations (DSOs); and local government officials
A. Project design
a. Context and background
Mental health is one of the most ignored issues in Bangladesh. According to the National Mental Health Survey Report 2018, 18.7 per cent of adults in Bangladesh are affected by mental health problems. Among them, about 92 per cent are not seeking mental health support due to multiple reasons, such as the scarcity of mental health professionals, high costs of treatment and social stigma. The budget allocated for mental health service provision is limited. Persons facing mental health problems do not want to share their distress and mental issues, fearing being stigmatized.
Due to societal barriers, persons with disabilities are more prone to mental health challenges. The limited mental health services are broadly not accessible. Persons with disabilities also face further stigmatization if they have mental health needs, and the community members and service providers have a limited understanding of disability issues.
The COVID-19 pandemic has taken a heavy toll on the mental health of people in Bangladesh, irrespective of age, gender and socioeconomic status. Among various populations, persons with disabilities are more likely to experience difficulties accessing mental health services. In this context, CDD implemented this project with OPDs and DSOs to promote a sustainable, replicable and scalable inclusive mental health service model at the community and national levels.
b. Objective and expected outputs
Objective: To promote inclusive community-based mental health services for persons with disabilities in Bangladesh to protect their mental well-being in the context of the COVID-19 pandemic.
Outputs:
- Increased availability of multi-tier inclusive mental health services for persons with disabilities at the community level;
- Strengthened capacity of OPDs and DSOs to provide inclusive community-based mental health services for persons with disabilities;
- Integration of inclusive community-based mental health services for persons with disabilities in public policy and programming.

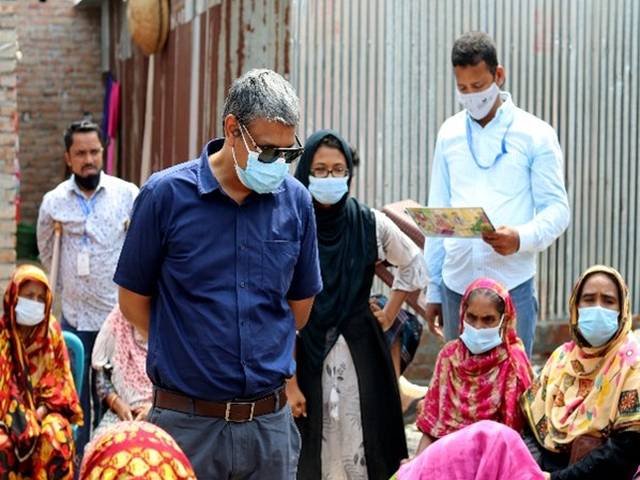
Training of peer responders
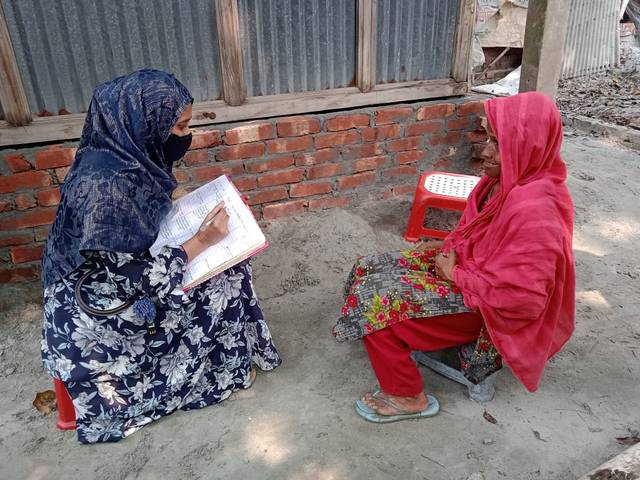
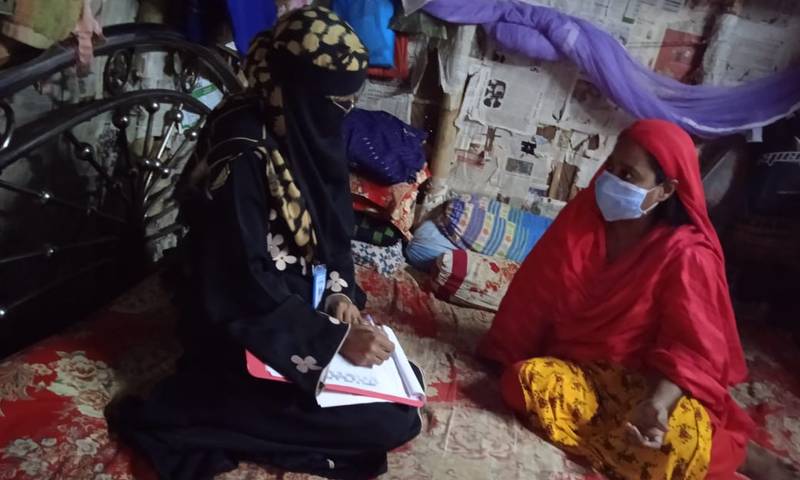
Home visit by peer responder
c. Partnerships
The project was implemented across Bangladesh in ten catchment areas in partnership with six OPDs and four DSOs. The main role of the partner organizations was to put into practice the concept of inclusive community-based mental health services in the project locations. They supported CDD in identifying and recruiting persons with disabilities as peer responders, monitoring project activities at the field level and contributing to the development of advocacy initiatives. The partner organizations also assisted peer respondents in providing mental health services, organized health camps, conducted advocacy campaigns and facilitated policy discussions with relevant stakeholders.
B. Achievements and lessons learned
a. Impact and results
Provision of inclusive mental health services for persons with and without disabilities
- A total of 20 peer responders (7 men and 13 women), including 14 persons with disabilities, were recruited and trained under the project. Being part of the project, they became empowered and developed their skills to respond to the primary mental health needs of community members.
- A total of 2,193 persons (1,018 men and 1,169 women), including 1,175 persons with disabilities, received mental health support from peer responders.
- A total of 778 persons were referred to nearby hospitals, including the National Institute of Mental Health (NIMH), for better mental health treatment. Among them, 304 persons (39.07 per cent) visited the hospitals and sought advanced services relating to mental health.
- A total of 229 persons received advanced mental health services from expert psychologists.
Increased awareness of community members, OPDs and policymakers on mental health issues
- Twelve community-level mental health consultation camps were held, and a total of 398 persons were assessed and diagnosed, including 320 persons with disabilities. Community members were briefed on the importance of seeking psychiatric support when needed.
- Training on inclusive community-based mental health programming and technical support visits were organized for 12 managers and 12 field staff of 6 OPDs and DSOs from different locations in Bangladesh.
- An advocacy plan and a policy brief were developed with the engagement of OPDs to integrate the concept of inclusive community-based mental health services into policymaking and programming.
- Three advocacy meetings at the national and local levels were held for representatives of the National Institute of Mental Health and local governments. They were sensitized to the significance of addressing the mental health needs of persons with disabilities in government services and incorporating community-based mental health into the Action Plan of the National Mental Health Strategy 2020-2030.
- One exposure visit to a pilot location was organized for government representatives. Another exposure visit was organized for representatives from World Health Organization (WHO) headquarters, WHO Regional Office for South-East Asia and WHO Bangladesh. They were informed about project interventions and services required by persons with mental health needs.
- A national-level dialogue on inclusive community-based mental health programming was organized to facilitate the integration of services for persons with disabilities into the Action Plan of the National Mental Health Strategy 2020-2030. The national-level workshop was participated by a total of 82 representatives from the Government and non-government bodies, including the Line Director of the Non-Communicable Disease Control (NCDC), Directorate General of Health Services (DGHS) and National Institute of Mental Health (NIMH) representatives.
This project prioritized women with disabilities in each area of its interventions.
- More than 50 per cent of peer responders were women with disabilities, contributing to women’s empowerment. The service delivery time was made suitable for women peer responders with disabilities, so they did not face any difficulty in providing services to others.
- Family members were more aware of the mental health needs of women with disabilities and supported women in developing skills to become peer responders. Services provided by women with disabilities were widely accepted by their peers.

Community awareness-raising meeting

Awareness session for caregivers
b. Challenges
During project implementation, measures were taken to address the following prominent challenges:
- Prevalent misconceptions and stigma about mental health in the community: Local government representatives, school teachers and community members were sensitized to mental health issues through regular court-yard meetings.
- Reluctance of persons requiring mental health support to see psychiatrists in the hospital: Peer responders made regular follow-ups with them to emphasize the importance of taking treatment. Persons requiring mental health support were invited to mental health camps organized in communities where they could talk to psychiatrists.
- Lack of financial resources to purchase required medicine for treatment: Peer responders informed persons in financial difficulty of the sources of free medicine. Regular counselling also helped them understand the importance of taking prescribed medicine.
- Difficulties in conducting in-person activities due to the pandemic: Peer responders conducted regular follow-up activities over the mobile phone (teleservice).
- Shortage of awareness-raising materials and tools: The existing materials already developed under other projects of CDD were utilized to ensure effective project implementation.
c. Sustainability
- Peer responders of this project have become skilled and confident in serving the community. They are capable of continuing these services in their respective areas.
- Persons with mental health needs and their family members in the project locations have been sensitized to mental health issues. In addition, they have better information about available government and non-government mental health services.
- Other projects of CDD with mental health-related activities will further promote the practice of recruiting peer responders. The strengthening of community-based mental health services will help meet the mental health needs of persons with disabilities and other marginalized groups in different locations.
- The capacity of OPDs and DSOs in inclusive community-based mental health programming has been increased. They have developed a better relationship with relevant mental health service providers. All these will allow OPDs and DSOs to continue their initiatives on mental health at the community level.
- The advocacy initiative will be continued by CDD and OPDs to influence public policymaking and programming on inclusive community-based mental health services.
- An accessible online knowledge hub has been developed to enhance knowledge dissemination, comprising resources on inclusive community-based mental health programming. These resources will be utilized by a variety of stakeholders to support community-based mental health services.

Advocacy meeting with local government officials
Exposure visit by government representatives

Exposure visit by WHO representatives
d. Good practices and lessons learned
-
Peer responding is an effective strategy to ensure inclusive community-based mental health services: Empowered peer responders with disabilities are self-advocates for disability rights and inclusion. They can reach out to persons with disabilities in need of mental health support and provide primary services.
Peer responders selected among persons with disabilities can easily recognize the needs of persons with disabilities as they are likely to have similar issues and concerns. They can fully understand the societal and environmental barriers, as well as financial hardship, experienced by persons with disabilities and can thus effortlessly empathize with their peers.
On the other side, persons with disabilities also trust peer responders with disabilities and feel comfortable communicating openly with them.
-
Mental health is critical for social well-being: If persons with mental health needs can speak up and share their issues with reliable people, they become more confident in managing their stress.
Persons who received mental health services through this project have been empowered to make independent choices and changes in their lives. For example, Salma (not her real name, aged 26) was mentally devastated after her divorce and suffered both socially and financially. She had suicidal thoughts due to her mental conditions. Peer responders recognized her issues and extended mental health support, which resulted in a positive change in her life. Salma is now referring people from her community to mental health services.
C. Feedback and resources
a. Voices of participants
“I thought that everything was lost, and I had no hope for my mother and myself. After receiving mental health services, I learned to think positively. I will try my best to support my mother and myself.”
---- Tuhin (aged 22) lives with a visual disability. He experienced a difficult situation due to his disability and suffered from mental health issues after his father’s death.

“The peer responder training boosted my confidence. I can address my own mental health issues now. Previously, I often thought about committing suicide even after knowing that committing suicide was not right - I could not find alternative options. Now I have more options to choose from to make my life meaningful.”
---- Shanta (aged 23) is a peer responder with a physical disability and lives with her mother. She faced a financial crisis and was depressed with suicidal thoughts.
“Now I have dreams, and I want to fulfil these dreams. I want my daughter to be educated and to live a quality life so that she will be able to fulfil all her dreams as well.”
--- Fatema (aged 26), single mother. She received support from peer responders.

b. Resources
- Knowledge Hub on Inclusive Community-Based Mental Health Services (in Bengali): https://cdd.org.bd/2021/09/05/mental-health/
- Policy brief, Inclusive community-based mental health services (ICMHS): https://cdd.org.bd/wp-content/uploads/2022/03/Policy-Brief_ICBMH-_CDD.pdf
- Presentation at ESCAP’s Regional Forum on Advancing Disability-Inclusive Development: Leadership and Participation of Persons with Disabilities toward an Inclusive, Accessible and Sustainable Post-COVID-19 World: https://www.unescap.org/events/2021/regional-forum-advancing-disability-inclusive-development-leadership-and-participation#